

Obsessive Compulsive Disorder Clinic

Content and trigger warning
This website contains information on OCD including examples of obsessions and compulsions. Some individuals may find reading these topics distressing. If you feel distressed by content on this webpage please press the 'Need help urgently' button on the top right of this webpage which can signpost you to support.
You don't need a formal diagnosis of OCD to access the information or support on these pages.
What is OCD?
Obsessive Compulsive Disorder (OCD) is a condition where people experience unwanted, intrusive and unpleasant thoughts and/or compulsive behaviours.
This experience can often be applied to an OCD cycle such as below. Here, people experience intrusive thoughts or feelings, which can become obsessive thoughts through applying an inflated sense of importance: this causes the individual to feel distressed. There are lots of examples of obsessive thoughts - please see ‘Obsessive thoughts’ below for more information. As a response to this feeling, individuals may carry out mental and physical compulsions, please see ‘compulsions’ below for more information. Although these may bring individuals temporary relief, this causes the cycle to be quickly repeated.
Obsessive thoughts are repeated and unpleasant intrusive thoughts, images or urges that pop into our minds involuntarily. Everyone experiences intrusive thoughts, but people with OCD can become preoccupied with these thoughts. This is because worry and attention can make these thoughts feel meaningful. Obsessive thoughts are always around things that you do not want to happen, or are fearful of happening. You may feel responsible for causing or preventing these things from happening, and you may engage in compulsions to reduce this anxiety. Intrusive thoughts are usually thoughts, but they can also be sounds, images, smells or sensations. Watch a video with some more information here, including examples of obsessions you may be experiencing
Compulsions are the things we do to try and stop obsessive thoughts from coming true and to get relief from the anxiety we may feel. These compulsions are often repeated many times and can take several hours each day. Common examples of compulsions can include checking (e.g. checking doors, electrical equipment) and cleaning (e.g. hand washing), asking for reassurance, and avoiding situations. Watch a video with some more information here, including examples of compulsions.
Avoidance is something you may find yourself doing to reduce exposing yourself to potential triggers. For example, if your obsessions are around the thought that you might hit a person with your car, you may avoid using your car or leaving your house. Watch a video with some more information about avoidance.
The OCD Cycle
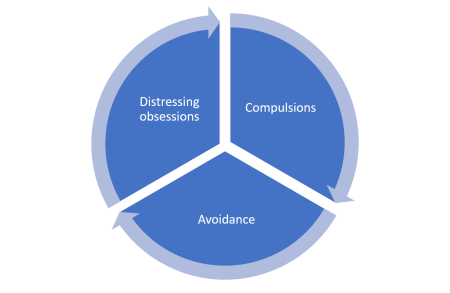
You may find it helpful to refer to the image of the cycle above.
The OCD cycle is an attempt to explain what is happening when a person with OCD experiences an intrusive thought. Not everyone experiences OCD in the same way. For more information on this, please see our short guide to the OCD cycle.
First, the person will encounter a trigger. These triggers will be different for everyone. For example, some people may be triggered by touching something, going outside or getting in their car. The person will then experience an intrusive thought, image or urge. Examples and more information can be found here. Watch a video with some more information including examples of triggers.
Lots of people without OCD experience intrusive thoughts. Clark and Purdon (1992, insert link) for example, found around 50% of people have thoughts that they have hit an animal or person with their car. However, those with OCD give these thoughts important meanings, and will experience unpleasant feelings such as guilt, anxiety and uncomfortableness.
As sitting with these feelings are uncomfortable, you may have urges to carry out certain behaviours to either stop the bad thought from coming true or to soothe how you are feeling. These behaviours are called compulsions. Here, we can see how the distressing obsessions can lead to compulsions. Carrying out these compulsions stops us from finding out if the meanings we have given the intrusive thoughts are true. See more information on this, including examples here. Carrying out these behaviours will give the individual temporary relief which, due to negative reinforcement, will increase their want to do it again.
Additionally, the person may avoid triggers to avoid the unpleasant feelings. See more examples and information here.
View our short guide on understanding the OCD Cycle.
Below is a video of Sophie Ward, a psychological wellbeing practitioner, explaining the OCD cycle in more depth.
Find out more about how to refer yourself.
The OCD Clinic, established in 2013, is for adults experiencing difficulties with OCD, whether the problem is mild or very severe. We offer high-quality evidence-based help, according to each person's need, based on the latest research and NHS guidelines.
Therapies on offer include supported self-help using Cognitive Behavioural Therapy (CBT) principles and workshops.
The OCD Clinic is part of the adult primary care mental health services in East Sussex (Health in Mind) and in Brighton and Hove (Brighton and Hove Wellbeing Service). The service also operates in some, but not all, of the Assessment and Treatment Services (ATS) in Sussex Partnership NHS Foundation Trust. If you are currently receiving care in an ATS in Sussex and are interested in accessing the OCD Clinic please speak to your Lead Practitioner to see if it would be possible to access through the psychological therapy service within the ATS
Although CBT is helpful for the majority of people who have OCD, not everyone will benefit. A third to a half of people find that CBT does not help to address their OCD symptoms. To improve care for people with OCD we are involved in a number of research projects. Clients attending the clinic will be offered the opportunity to take part in these projects if they wish to, however, this is entirely optional.
The OCD Clinic was established by Professor Clara Strauss, consultant clinical psychologist working in the Research and Development department at Sussex Partnership NHS Foundation Trust.
What support is available?
Find out more about how to refer yourself.
Up to one million people in the UK live with some form of OCD. Although most people with OCD know that their compulsions can be excessive, they nonetheless feel unable to control their thoughts or their behaviour. Fortunately, there are well-established and effective ways of helping. The National Institute of Health and Care Excellence (NICE) recommends cognitive behaviour therapy (CBT) for OCD. At the OCD Clinic, the particular type of CBT we use to tackle OCD is known as Exposure and Response Prevention (ERP).
How does Exposure Response Prevention (ERP) work?
ERP is an evidence-based therapy which is aimed at breaking the cycle of obsessive thoughts and compulsions which make up OCD. During ERP, you will expose yourself to a range of different situations which bring on your obsessive thoughts or compulsions, whilst at the same time resisting the urge to carry out your compulsions. Over time, your anxiety will reduce naturally without the compulsion: this reduces the strength of the link between your obsessive thoughts and your compulsions. Whilst ERP exercises can be difficult, they generally become easier the more you do them and you will be allowed to build up your confidence throughout the process. Your ERP will also be undertaken with the support of a trained practitioner, who will help you to devise a plan and carry out the exercises in a systematic way. In the OCD clinic, the recommended way to do this is in group therapy.
Find out more about CBT, see 'What can I expect from the clinic'.
For more information on support, please see our short guides to exposure and response prevention and group therapy.
Please see here for information on how to access support, including who can access support and what to expect.
The OCD Clinic is part of Sussex Partnership's adult primary care mental health services in Health in Mind (East Sussex), Brighton and Hove Wellbeing Service and Brighton and Hove Assessment & Treatment Service.
If you are experiencing OCD difficulties and would like help please speak to your GP about a referral to the OCD Clinic.
You are also very welcome to refer yourself directly to the OCD Clinic, please see below on how to do this based on location.
East Sussex (Health in Mind)
If you live in East Sussex you can refer yourself directly via Health in Mind, a free NHS Service for those experiencing emotional or psychological difficulties. Self-referrals can be made through telephone: call 03000 030 130 and ask to be referred to the OCD clinic.
Alternatively, you can complete an online self-referral form on the Health in Mind website: click here to access the self-referral form. On the form it will ask you to state “What are your current difficulties as you see them?” In this box please state that you would like to be referred to the OCD clinic
Brighton & Hove (Brighton & Hove Wellbeing Service)
If you live in Brighton and Hove you can also refer yourself directly via the Brighton & Hove Wellbeing Service. Simply complete an online self-referral form and state that you would like to be referred to the OCD clinic: click here for the self-referral form.
Brighton and Hove Assessment and Treatment Service (ATS)
Whilst there isn’t a self-referral option for those trying to access the OCD Clinic through the Brighton and Hove ATS, those who are open to the service and who are interested in accessing support should speak to a clinician working in this service who is directly involved in their care. A clinician will then be able to make a referral to the OCD Clinic on your behalf.
Please note we cannot accept referrals through to the following contacts but you can find out more about referrals here.
Email: SPNT.OCDClinic@nhs.net
Address: OCD Clinic, Research and Development, Sussex Education Centre, Mill View Hospital Site,
Nevill Avenue, Hove BN3 7HZ.





