Frequently asked questions (FAQs)
You may have some questions about Sussex Gender Service so we've pulled together some frequently asked questions here:
We are an NHS adult gender service pilot in Sussex, which has been commissioned to provide local transgender healthcare for trans and non-binary people. This includes assessment and diagnosis for gender incongruence which involves a holistic assessment of an individual's needs and offers referrals and signposting to other services.
Sussex Gender Service is staffed by an experienced multi-disciplinary team and receives clinical support from the gender identity clinic at Nottingham Centre for Transgender Health. We have care navigators with lived experience that work with people who access our services to provide support and help with connections to local organisations.
The service has been commissioned by NHS England to run as a two-year pilot. After two years NHS England may wish to extend the pilot for a further year.
Sussex Gender Service follows the same service specification from NHS England as other gender service pilots, which is similar to the existing gender identity clinics. This means we follow the same assessment process and offer the same treatment pathways, and in some circumstances, this will be provided by Nottingham Centre for Transgender Health. However, it is important to us that we develop and provide a service that is unique and tailored to people living in Sussex. We are working closely with the community to understand what service users want to see from our service.
Sussex Gender Service will see patients aged 17+ who are registered with a GP in Sussex and are already on a waiting list for one of NHS England’s seven national gender identity clinics.
Patients will be given a choice to remain where they are, on the original gender identity clinic waiting list, or be seen by the new service, which will start seeing patients from October 2023. Patients will be contacted by the Sussex Gender Service to confirm what choice they would like to make.
Transferring to the new service will likely mean that you are seen closer to home in a timelier way, whilst maintaining full access to all the services of a gender identity clinic as we are working in partnership with the Nottingham Centre for Transgender Health.
It's anticipated that by transferring to Sussex Gender Service you'll be seen sooner than by remaining on the original gender identity clinic waiting list, as the Sussex Gender Service will only be seeing patients from this region.
However, you should check with the original gender identity clinic about where you are on their list, and the length of time to your first and second assessments, if you were to remain with them. If you agree to be transferred to Sussex Gender Service, you will be offered a first assessment to be seen based on your original referral date at your originating gender identity clinic.
The waiting list of patients is based on the date of referral by the GP to the original gender identity clinic. You will be contacted and offered an appointment based on who has waited the longest, no matter to which clinic you were originally referred.
You are unable to be moved higher up the list, as it is based on who has waited the longest time. We believe this is the fairest approach to all patients and this is the same process across all gender service pilots and gender identity clinics.
It's your choice. You don't have to transfer to Sussex Gender Service; you can decide to remain on the gender identity clinic list that received the referral, or transfer to our service. You will be contacted and given a choice to move to this service or stay where you are.
If you decide not to transfer to Sussex Gender Service, then we will advise the relevant gender identity clinic that you want to stay on their list and be seen by them.
Yes. As long as you have not already attended your first appointment at the gender identity clinic, you can change your mind. It is only once you have been seen by the gender identity clinic for your first assessment, that you no longer have the option to transfer to Sussex Gender Service.
Based on information that we have from other gender service pilots this is very unlikely to happen. Other Pilot sites have seen everyone on their initial waiting lists. However, if this did happen then you would be transferred to the gender identity clinic service or waiting list that you were originally placed on.
We will always seek your consent to access any mental health records.
No, only patients on the waiting list are eligible to transfer. As your assessment and treatment has already started you will need to stay with the gender identity clinic who is assessing you.
St Peter's Health Centre, 30-36 Oxford St, Brighton, East Sussex, BN1 4LA.
The Sussex Gender Service is led by Sussex Partnership NHS Foundation Trust with clinical oversight and specialist support provided by Nottingham Centre for Transgender Health, one of the seven established gender clinics operating across England. In some circumstances people will be seen by Nottingham Centre for Transgender Health. The service has been commissioned by NHS England.
We will begin to contact patients on the waiting list mid-September and will start offering appointments from the beginning of October. We anticipate by the beginning of January 2024 our staff team will be fully recruited and we will be able to start operating at full capacity once our teams have been fully trained.
Sussex Gender Service is a pilot which means after two years NHS England may wish to extend the pilot for a further year, subject to an independent evaluation of the service. Following the evaluation NHS commissioners will decide on future provision of gender services in this area.
You can access the service if you are already on a waiting list for one of NHS England’s seven national gender identity clinics and registered with a GP in Sussex.
At this point Sussex Gender Service is not able to take new referrals into our service, either from individuals or GPs.
People who wish to be referred to gender services should speak to their GP first and request a referral to one of the national gender identity clinics.
No, because the service is a pilot we are only taking existing referrals from other gender clinics.
When you are contacted by Sussex Gender Service you will be sent a pre-appointment form which asks you some information ready for your first appointment.
You will be offered two assessment appointments. The time between these appointments will be between six weeks to three months.
At the end of the second appointment some people will be given a diagnosis of gender incongruence and information about our therapy pathways.
Other people may need some further appointments to help them work out the best options and pathways.
People can choose to access as few or as many therapy pathways as they like. Our clinicians will help support you to understand these pathways and how and whether you can access these different therapies.
We also have care navigators working in our service. They are people who have lived experienced who can help support you with your journey and link you in to other relevant services and groups in the community.
We will start seeing patients in October 2023 using a blended model of video consultation and face to face appointments, based on clinical need, patient digital access, and patient choice.
If you need to travel to be seen, and you are on low income or benefits, you can re-claim travel expenses.
More details about reclaiming travel expenses are available here.
Claims will need to be made using the form provided on the NHS.uk website. We are unable to reimburse any costs at the clinic as we don't have a cashier’s office.
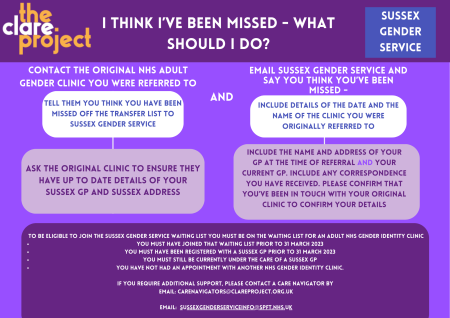
There could be a number of reasons why the service hasn't been in touch.
We are taking patients onto our waiting list in batches. We will contact patients in order of referral date.
If you think you are eligible (because you're registered with a Sussex GP surgery, and are on an existing gender identity clinic waiting list, and were originally referred before 31 March 2023) contact your originating clinic to see if your details have been shared with us.
The service is setting up at the moment so we don't know this at this stage. We will update this when we know more. Our aim is to see people as quickly as possible.
Sussex Gender Service is commissioned by NHS England to deliver treatment and recommendations that follow the service specification and we will need to undertake the assessment process. However, your care plan will be individual to you, based on your needs, and agreed between you and one of our clinicians. We will consider where you are on your journey, including previous diagnosis and treatment.
Our staff are trained to make sure they know about the Data Protection Act and their legal responsibilities to keep your information safe.
As with any NHS service we take great care to ensure information about you stays secure. Confidentiality is a key component to running the service. Anyone who receives information from us is also under a legal duty to keep it confidential.
Yes, if you decide you want to be seen by Sussex Gender Service, an appointment letter will be sent to you. After your appointment we will send you an appointment outcome letter and send a copy of this letter to your GP.
GPs receive copies of most letters sent to the patient to ensure they have the necessary clinical information they may need.
Transgender awareness sessions are being held for GPs across Sussex. These sessions will give an overview of transgender health, the patient pathway within a gender service, and outline the role of clinicians and how the service operates. These sessions will also look in detail at the advice, support and guidance given to patients and GPs while a patient is being seen at the service.
Sussex Gender Service has experienced clinicians who can help support you with your mental health.
Sussex Gender Service has clinicians who are experienced in working with people who are intersex. In addition, the service receives specialist supervision and consultation from the Nottingham Centre for Transgender Health.
The best thing to do is to speak to your GP. You can also contact one of the specialist organisations listed in our resources and information section for further help and support.
The term currently used to describe a discrepancy between birth-assigned sex and gender identity is gender incongruence.
Gender incongruence is frequently, but not universally, accompanied by gender dysphoria.
Gender dysphoria is the discomfort or distress felt by experiencing a discrepancy between birth-assigned sex and gender identity. In order to access transgender healthcare treatments, it is necessary to obtain a diagnosis of gender incongruence or gender dysphoria.
To access the therapy pathways, we offer a diagnosis of 'gender incongruence and dysphoria' at your second assessment.
'Incongruence' means a mismatch between your gender assigned at birth and your experienced gender.
'Dysphoria' means the state of unease, unhappiness or dissatisfaction due to gender incongruence.
People interpret these words in different ways, and no words will be a perfect fit for everyone. Some people don't like to have a diagnosis at all. To access gender-affirming NHS therapy, such as surgery, a diagnosis of gender dysphoria is required, because experiencing dysphoria (unhappiness and unease) explains why people need the NHS therapies we offer. The aim is that by offering treatments to help with dysphoria, people will feel 'congruence' (harmony) with themselves.
Having the words 'gender incongruence and dysphoria' can also be helpful to have in a clinical letter for some people, in case you want to use our official clinic letter for documentation or evidence of attending our service in the future.
We offer the same diagnosis to everyone but we are aware that these can be felt differently by different people. The most important thing is how you feel, and the care you receive - we will always want to focus on your individual and personalised care and strive for the best outcomes for you.
There is no check-list which we use in Sussex Gender Service, but instead we have a conversation about your lived experience of gender, and how you would feel accessing gender-affirming therapy, or how you feel about the therapy you might have already received. There is no requirement for you to have socially transitioned, or changed your name, or anything else, for us to offer you a diagnosis.
We'll ask questions such as how you feel about the gender you were assigned at birth and how this matches (or mismatches) how you feel now. We'll ask about your therapy goals within the service. We may also check your understanding about benefits or drawbacks of specific therapies you would like to access (such as hormone therapy).
When you have your assessments, there are no trick questions. We just want to make sure we offer the right therapies and the right times to ensure your best outcomes. It might be that you are offered a diagnosis of gender incongruence and gender dysphoria, but do not want to access therapies such as hormones or surgery currently. In this case, we can chat about the best way forward, and it may be that you choose to be discharged back to the care of your GP, and re-referred when you feel ready.
At the end of your second assessment, if we are still not sure that what you are experiencing is gender incongruence and dysphoria, we might offer you extra appointments with a gender specialist psychologist to explore in depth what you are experiencing and how we can best support you. We provide a safe space to talk with a regular clinician over the course of several sessions.
If you have any more questions or feedback about this, please email the team or discuss with your Gender Clinician during an appointment.
Care navigators are trans, non-binary or intersex (TNBI) community members who work alongside Sussex Gender Service to offer you help and advice. The role is still under development and welcomes your feedback, but the aim is to support you as you journey through the service pathways and help you access information about the Sussex Gender Service. They can support you with a variety of issues while you are seen by the service, through group and individual support.
Care navigators are employed by The Clare Project and work closely with the Sussex Gender Service, but are independent of the NHS.
You can find out more about care navigators and find a form to refer yourself for their support:
Find out more about care navigators here, or email carenavigators
Sussex Gender Service is a partnership with Sussex Partnership NHS Foundation Trust and Nottinghamshire Healthcare NHS Foundation Trust (Nottingham Centre for Transgender Health network) to deliver link clinic provision.
This will ensure that you have the same access to the treatment and support as you would if you remained at the originating gender identity clinic.
This also ensures that experienced gender specialist clinicians are there to support the development of the new service, and to provide additional support for any complex assessment or treatment needs you may have, along with surgical recommendations for genital surgery.
Listening to and learning from feedback helps us to improve our services and make sure we provide the highest quality care and treatment.
You can talk directly to your care team, or you can share feedback about the service via the Sussex Experience Survey, or by contacting the Patient Advice and Liaison Service.
We are also developing further ways people can provide feedback on the service which we will share when details are available.
If there are issues regarding your mental wellbeing, then please contact your GP surgery or local mental health service, if you are already been seen by them. If the matter is urgent then see our help in a crisis page, contact 111, or your GP surgery.